Diseases of the Veins
Diseases of the Veins
Venous disorders are classified as conditions that damage the veins in your legs leading to chronic venous insufficiency. The veins in your legs are responsible for transporting blood back to your heart using valves to prevent backward blood flow into your ankles or feet. Damage to these valves can cause venous incompetence leading to increasd blood pressure in the veins in your legs which may cause serious complications and put your overall health at risk.
At 901 Vascular, our specialists can diagnose and treat all venous disorders, providing comprehensive care and relief from symptoms. Learn more about various venous diseases and their available treatment options.

An ultrasound scan is the only definitive way to diagnose vein disease. A technician uses this test to take an image of the inside of the veins in your leg. A qualified medical doctor will review the test results to determine if the valves inside the veins are working properly.
Varicose veins and chronic venous insufficiency (CVI) are recognized by many insurance companies, including Medicare and private insurers, as treatable medical conditions.
Varicose Veins
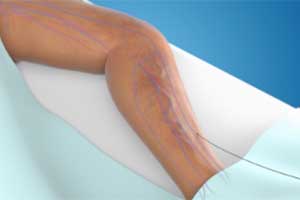
Varicose veins are large, raised blood vessels that commonly appear on the inner legs or in the lower pelvic region that are caused from the increased blood pressure in the veins in your legs. These superficial veins can be seen through the skin in a bulging, bluish-purple hue. While varicose veins themselves are not a threatening medical condition, they can be uncomfortable and even painful to some individuals. Venous disease can worsen over time and to treat progression would require professional treatment.
Varicose veins are not just a cosmetic issue.
Vein disease in the legs can cause varicose veins and other painful symptoms that can impact how you live. We believe life shouldn’t be limited by pain caused by leg vein disease, and that’s why we’re here to help you understand your pain and break free from it.
Common signs and symptoms of venous disease
-
Aching or pain in legs
-
Swelling of legs or ankles
-
Cramping
-
Heaviness or tiredness
-
Itching, sores, or ulcers
-
Restlessness
-
Skin changes and/or darkened calf discoloration
-
 Skin Color and Texture Changes*
Skin Color and Texture Changes* -
 Leg Swelling*
Leg Swelling* -
 Varicose Veins*
Varicose Veins*
-
Known risk factors
- Family history
- Smoking
- Current or previous pregnancies
- Obesity or excess weight
- Prolonged sitting or standing
- Leg injury or trauma
- Lack of exercise
- A blood clot (deep vein thrombosis)
-
Causes of leg vein disease
There are a number of factors that can put an individual more at-risk for developing varicose veins. Some of these include:
- Obesity
- Personal history of peripheral venous disease
- Family history of blood clots
- Family history of varicose veins
- Hormonal changes (Through pregnancy, puberty, or menopause.)
- Previous skin injury/surgery
Spider Veins
Similarly to varicose veins, spider veins are very superficial blood vessels that can be seen directly under the skin. These veins have a red or bluish hue and can be uncomfortable or cause itching. Spider veins affect only the capillaries, the smallest blood vessels in the body, and typically appear on the legs or face.
Varicose veins are not just a cosmetic issue.
They can occur with varicose veins or be a solitary skin issue without a medical venous disease accompanying the spider veins. They can occur due to a family history of spider veins, in response to weight gain such as pregnancy, or in response to skin injury/surgery.
While both varicose and spider veins can be uncomfortable, most complaints of pain come from patients suffering with symptomatic varicose veins. These swollen blood vessels are larger than spider veins, causing cramps and aches in the legs. Additionally, varicose veins can cause swelling, ulcers. Less commonly, chronic venous insufficiency can lead to inflammation or superficial thrombus to develop in affected veins.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) occurs when a blood clot forms in a vein located deep in the body, typically in the lower legs, thighs, or pelvis. These blood clots may partially or completely block off the flow of blood in the legs and could potentially embolize other parts of the body such as the lungs and cause major problems. While on its own DVT is not life threatening, the potential for the clot to break loose and lodge elsewhere makes it a serious condition you must receive immediate medical attention for.
While DVT can occur without obvious symptoms, be aware of new swelling in the leg, leg pain, a change of color of the skin (red or purple), and or one leg acutely becoming larger than the other leg. These can all be signs that you are experiencing deep vein thrombosis and may need to speak to your medical provider for an evaluation.
DVT can be caused by anything that prevents blood from properly flowing back to the heart from the legs. There are several risk factors that can cause deep venous thrombosis to develop.
- Clotting Disorders
- Sedentary Lifestyle
- Previous leg injury or surgery
- Hormonal changes (Through pregnancy.)
- Family history of deep venous disease or pulmonary embolism
- Use of birth control pills
- Recent cancer treatment such as radiation or chemotherapy
Leg Ulcers
Similarly to varicose veins, spider veins are very superficial blood vessels that can be seen directly under the skin. These veins have a red or bluish hue and can be uncomfortable or cause itching. Spider veins affect only the capillaries, the smallest blood vessels in the body, and typically appear on the legs or face.
Early diagnosis is critical
When left untreated, leg vein disease can progress into a more serious condition known as Chronic Venous Insufficiency. If CVI is left untreated, legs can sometimes develop painful sores or wounds on the skin’s surface, called ulcers. Ulcers typically appear near the ankle or lower leg and are brought on from the increased buildup of fluid and blood pressure from veins affected by CVI.
A venous leg ulcer is a chronic sore that takes more than two or three weeks to heal and is caused by increased venous pressure in the legs. Unlike typical cuts and scrapes, these ulcers may not heal without proper treatment and may also cause discolored skin around the wound, or give off discharge. While they are not life-threatening, there is always a risk for infection and further complications. Leg ulcers may also come back repeatedly if the underlying issue is not addressed.
Venous leg ulcers can also form if you have previously or currently experienced varicose veins.

Venous Leg Ulcer*
Patients who receive early vein closure treatment along with compression stocking therapy for venous leg ulcers experienced significantly shorter time to healing and extended time free from ulcers.
- More than one million people in the United States suffer from venous leg ulcers.
- 70-90% of ulcers below the knee are venous (caused by vein disease).
- More than 50% of venous ulcers treated are recurrent ulcerations.
- Due to pain, mobility limitations, and other consequences, venous leg ulcers have been associated with increased rates of depression and substantial decreases in patient quality of life.
Treatment Options
While many of these afflictions have no concrete cure, there are several treatment options to reduce inflammation and appearance. Compression stockings are a conservative treatment option utilized by practitioners to reduce overall swelling and discomfort but they do not treat the vascular source but can help relieve symptoms of chronic venous insufficiency.
Sclerotherapy
While these passive methods can eventually help lower the visual appearance and pain of varicose veins, there are also procedures that can minimize symptoms more rapidly. For one, sclerotherapy is a minimally invasive procedure where a solution is injected directly into the veins. This solution scars the interior of the spider vein or varicose vein, causing it to eventually collapse and fade from view once absorbed by the body naturally. Blood is then naturally rerouted through the healthier veins through competent venous valves.
Venous Laser Ablation
Additionally, patients can undergo venous laser ablation. Much like sclerotherapy, this procedure is minimally invasive. After the skin is numbed, a small wire is inserted into the vein and delivers laser energy, sealing off the vein while remaining healthy veins continue to move blood around. After venous laser ablation, you may have some mild bruising around the treatment site, however these bruises will eventually fade and leave you with clearer legs and less painful veins.
ClosureFast Procedure
-

Step 1: Thermal catheter is placed
Using an ultrasound, your physician will position the catheter into the diseased vein through a small access site.
-

Step 2: Local anesthetic is applied
A series of injections numb the area around the vein that will be treated.
-
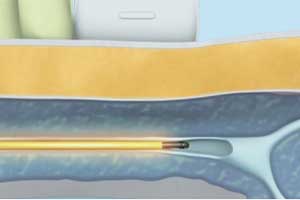
Step 3: Heat is delivered to vein wall
The vein wall is heated and the catheter is withdrawn from the vein.
-
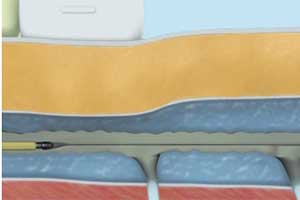
Step 4: Vein is closed
The vein is “heat sealed” as the catheter is removed. A multilayer compression wrap is applied from foot to groin post procedure.

Before The ClosureFast Procedure
You will have an ultrasound imaging exam of the leg being treated. This exam is important for assessing the diseased superficial vein and planning the procedure.
During the procedure
Your doctor will discuss the procedure with you. Here is a brief summary of what to expect:
- The ClosureFast procedure is performed on an outpatient basis. Your doctor will perform the ClosureFast procedure. Using an ultrasound, your doctor will position a catheter in the diseased vein through a small opening in the skin.
- The small catheter delivers heat to the vein wall, causing it to shrink and seal the vein. Once the diseased vein is closed, blood will reroute itself to other healthy veins.
After the procedure
- You will be taken to the recovery area to rest.
- Following the procedure, your doctor will apply a simple bandage over the insertion site and will give you compression stockings to aid in the healing process. Your doctor may encourage you to walk and to refrain from extended standing and strenuous activities for a period of time. The average patient typically resumes normal activities within a few days.1,2
- Your doctor will recommend follow-up care as needed.
Patient results: Before and After
-
 Before ClosureFast procedure*
Before ClosureFast procedure* -
 Six weeks after ClosureFast procedure*
Six weeks after ClosureFast procedure* -
*Individual results may vary. Images courtesy of Dr. Kathleen Gibson via Medtronic Venous Asset Image Library
Benefits of the ClosureFast procedure
- Relief of symptoms after two days, with a noticeable improvement in one to two weeks
- Minimally invasive outpatient procedure
- Less pain and bruising than laser treatment
- Faster recovery than laser treatment
- Proven results with positive patient experience
- Rapid recovery — on average, patients resume normal activities within a few days
- Lasting results — the only radiofrequency energy procedure with published long-term clinical data demonstrating safety and efficacy, with a 91.9% closure rate at five years.
Adverse events can include nerve injury, hematoma, phlebitis, thrombosis, and/or pulmonary embolism.
What type of therapy is ClosureFast
Thermal shrinkage of the vein wall with radiofrequency energy or heat
- Inpatient or outpatient procedure: Outpatient procedure
- One- versus two-leg treatment: Typically, each leg will be treated in separate appointments
- Needle sticks required: One needle stick for vein access. Typically, 5 to 10 needle sticks for anesthesia.
Typical post-treatment recovery
Healing of vein access site, anesthetic needle stick sites, and also healing of ablated vein section
- Compression hose: Required for approximately one week
- Procedure success rate: 91.9% after five years
ClosureFast procedure FAQ
Is the ClosureFast procedure painful?
Most patients report feeling little, if any, pain during the ClosureFast procedure.3 Your doctor will give you a local or regional anesthetic to numb the treatment area.
When can I return to normal activity?
Patients treated with the ClosureFast procedure may resume normal activity more quickly than patients who undergo surgical vein stripping or laser ablation. With the ClosureFast procedure, the average patient typically resumes normal activity within a few days.2 For a few weeks following the treatment, your vein specialist may recommend a regular walking regimen and suggest you refrain from strenuous activities (heavy lifting, for example) or prolonged periods of standing.
When will my symptoms improve?
Most patients report relief of symptoms after two days, with a noticeable improvement in one to two weeks.
Is there any scarring, bruising, or swelling after the procedure?
Most patients report limited to no scarring, bruising, or swelling following the ClosureFast procedure.3
How is the ClosureFast procedure different from endovenous lasers?
Both ClosureFast and lasers use thermal technology to deliver heat into the diseased vein, but they each use a different method of delivery. Despite their similarity in using heat, a 2009 study showed that the ClosureFast procedure is associated with lower rates of pain, bruising, and complications and a faster improvement in patients’ quality of life when compared to 980 nm laser ablation.4
How is the ClosureFast procedure different from vein stripping?
During vein stripping, incisions are made in the groin and calf, and a tool is threaded through the diseased vein to pull the vein out of the leg. With the ClosureFast procedure, only one small incision is made at the insertion site and the vein is then treated and left in place. ClosureFast is a minimally invasive approach that reduces the likelihood of pain and bruising, associated with vein stripping surgery.1
Is the ClosureFast procedure covered by insurance?
Many patients have access to the ClosureFast procedure through their insurance coverage plan. Insurance companies detail access to the ClosureFast procedure and other radiofrequency ablation procedures in coverage policies for varicose veins or chronic venous insufficiency. As with all healthcare procedures, you may also have some cost associated with receiving treatment, such as a copay or coinsurance. Please reach out to your insurance company to discuss your specific plan coverage and potential costs prior to seeking treatment
VenaSeal Procedure
-
Step 1: Catheter is placed in the vein
Using an ultrasound, your doctor will position a catheter into the diseased vein through a small access site. -
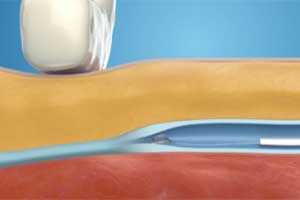
Step 2: Specialized adhesive is placed
A specially formulated medical adhesive is placed in the diseased vein via a small catheter. -

Step 3: Light external pressure is applied
Light external pressure is applied to adhere the vein walls together. This step is repeated for the length of the vein. -

Step 4: Catheter is removed
The catheter is removed and a single adhesive bandage is applied to the vein access site.
-
VenaSeal Live Procedure
-
VenaSeal Animated Procedure
Before The VenaSeal Procedure
You will have an ultrasound imaging exam of the leg being treated. This exam is important for assessing the diseased superficial vein and planning the procedure.
During the procedure
Your doctor can discuss the procedure with you. Here is a brief summary of what to expect:
- You may feel some minor pain or stinging with a needle stick to numb the site where the doctor will access your vein.
- Once the area is numb, your doctor will insert the catheter (i.e., a small hollow tube) into your leg. You may feel some pressure from the placement of the catheter.
- The catheter will be placed in specific areas along the diseased vein to deliver small amounts of the medical adhesive. You may feel a mild sensation of pulling. An ultrasound will be used during the procedure to guide and position the catheter.
After the procedure
- After treatment, the catheter is removed and a small adhesive bandage is placed over the puncture site.
- You will be taken to the recovery area to rest.
- Your doctor will recommend follow-up care as needed.
Patient results: Before and After
-
 Before VenaSeal procedure*
Before VenaSeal procedure* -
 Three months after VenaSeal procedure*
Three months after VenaSeal procedure* -
*Individual results may vary. Images courtesy of Dr. Kathleen Gibson via Medtronic Venous Asset Image Library







